By Debbie Gardner
debbieg@thereminder.com
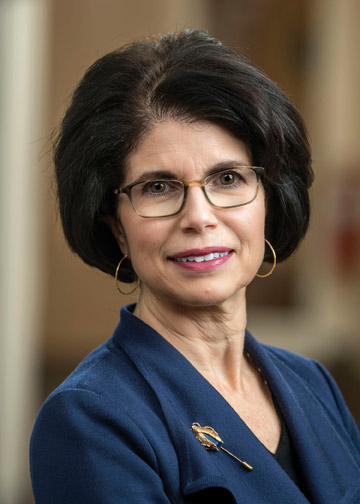
Dr. Grace Makari-Judson is co-director of The Rays of Hope Center for Breast Cancer Research and chair of the Baystate Health Breast Network. Here is what she shared with Prime about the latest in breast cancer treatments:
Q: The information on breast cancer detection is constantly evolving. What are some of the latest procedures for early detection and evaluation?
Mammography continues to be the gold standard for early detection of breast cancer and lowers the risk of death from breast by cancer by as much as 30%. Although mammography facilities were temporarily closed at the height of the pandemic, they have reopened with precautions being taken to keep women safe. Women should not use the pandemic as an excuse to skip screening. What we don’t want to see is an uptick in advanced breast cancer cases because women were afraid to come in.
When a breast problem is identified, ultrasound is extremely useful in further evaluation of an area of concern. Ultrasound may be used to screen women with dense breasts but has its limitations.
An MRI of the breast is most helpful in screening women at high risk of breast cancer, usually because of strong family history or known genetic risk. MRI is costly, requires at least 45 minutes to perform and requires an injection of a dye called gadolinium. A new type of breast MRI being investigated is called abbreviated MRI, takes only 10 minutes and is easier to interpret. A study published in JAMA Feb 2020 from the ECOG-ACRIN Cancer Research Group showed that abbreviated MRI was better than digital tomosynthesis (3-D mammography) in screening average risk women with dense breasts. Abbreviated MRI detected two and a half times as many breast cancers as mammography. We don’t yet know if abbreviated MRI is effective in reducing the risk of death from breast cancer. Additional studies are needed to consider the cost and feasibility of screening larger numbers of women since half of all women over the age of 40 have dense breasts. Abbreviated MRI is not yet available outside a research setting but we are following the studies with great interest.
Q: As detection methods evolve, so does treatment. What are some of the ways new research can direct the course of treatment for a patient?
Two important themes highlight the focus of clinical trials in breast cancer and include “precision medicine” and “de-escalation”. Precision medicine includes selecting the best treatment for a cancer based on the characteristics of the tumor and molecular profiling. For example, by looking at genes that are associated with rapid growth of cancer, we can estimate whether a cancer can be adequately treated with a hormone medication alone or requires the addition of chemotherapy. In patients with metastatic cancer, next generation sequencing of the tumor can identify specific targets for new treatments. This past year, there has been an unprecedented number of new drugs approved for advanced breast cancer.
De-escalation refers to looking at the effective treatments we have for early stage breast cancer and seeing if it is possible to have the same excellent outcomes with less treatment. A new clinical trial from ECOG-ACRIN offered at Baystate Regional Cancer Program is called the COMPASS trial. This is a trial specifically for women with a type of cancer that overexpresses HER2 neu where there are excellent drugs that can be given prior to surgery to shrink a cancer. Equally important is the ability to see the response of the cancer to the treatment, and then customize any needed additional treatment after surgery. Offering treatment that is less likely to lower blood counts and suppress the immune system is particularly appealing with concerns about COVID. De-escalation has also been an important theme in breast surgery and radiation to reduce possible late effects of treatment and still achieve high rates of cure.
Q: Breast cancer is more common in white women, yet the risk of dying is higher is black women? Why are there disparities in outcomes?
Black women may present with more advanced breast cancer and a more aggressive type of breast cancer known as triple negative breast cancer. Although multiple factors may play a role in poorer outcomes, including access to care, obesity and diabetes, one possible contributing factor may be the ability to tolerate certain chemotherapy drugs.
Chemotherapy is an important component of curative treatment. Black women are less commonly participants in clinical trials, so most of the information we have is based on studies of predominantly white women.
Those of us in health care, and in particular in breast cancer research, are invested in ending these disparities. A national study called EAZ171, from ECOG-ACRIN Cancer Research Group, is one of the first breast cancer trials focusing specifically on black women. The goals of this study are to identify which women are most susceptible to neurotoxicity from chemotherapy and which treatments would lead to best long term results. Neurotoxicity refers to side effects that cause numbness, tingling and pain in the hands and feet. When these side effects interfere with day to day activities, the doses of chemotherapy need to be reduced. This in turn may reduce the success of the treatment.
Neurotoxicity may be worse with certain chemotherapy drugs that are important in achieving cure. However, the same drugs may cause different side effects in different individuals. One of the goals of this study is to determine who is most susceptible to neurotoxicity based on inherited variability in breaking the drugs down. Predicting which drugs may be better tolerated in each individual can help to lower side effects, improve quality of life for breast cancer survivors and lead to better outcomes overall.
As of early September 2020, 367 sites have been approved to participate in the study. Baystate Medical Center is one of first 28 sites that has started enrolling patients. Results from this trial have the potential to change the standard of care for black women with breast cancer.